Bone Spur
Bone Spur
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview
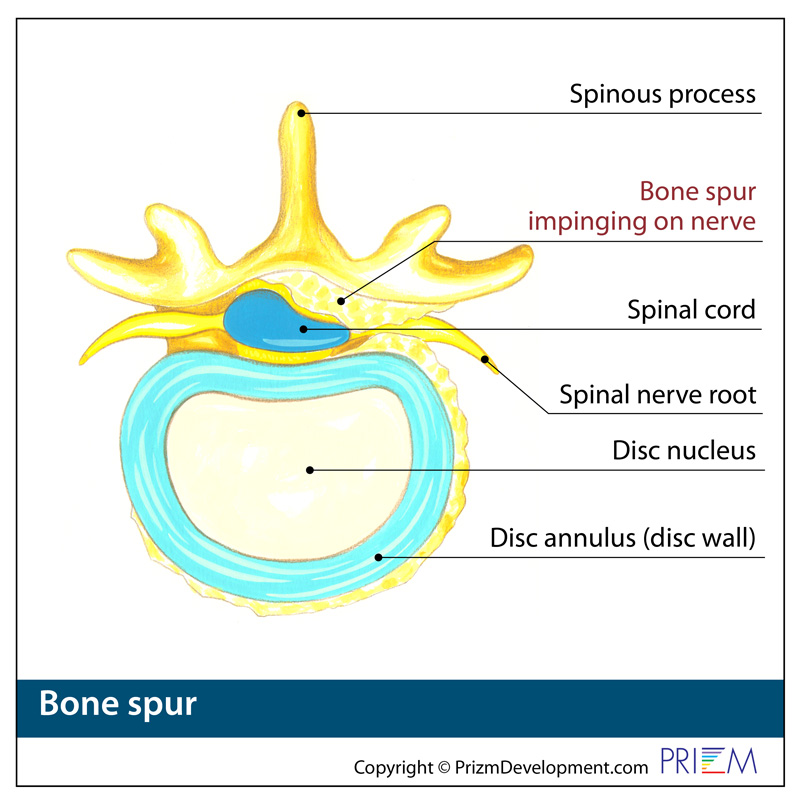
A bone spur, or osteophyte, is a projection of bone that develops and grows along the edge of joints. Bone spurs are fairly common in people over the age of 60. It is not the bone spur itself that is the real problem; pain and inflammation begin to occur when the bone spur rubs against nerves and bones.
Causes
As we age, the discs in our spine naturally degenerate and lose some of their natural shock-absorbing ability. Factors that contribute to and accelerate this process include stress, injury, poor posture, poor nutrition, and family history.
It is not uncommon for people with osteoarthritis to get bone spurs. Osteoarthritis is a degenerative condition in which joint cartilage begins to wear down, causing bone to rub against bone. As a result, the body may begin to produce new bone to protect against this, which is how a bone spur forms.
[top]
Symptoms
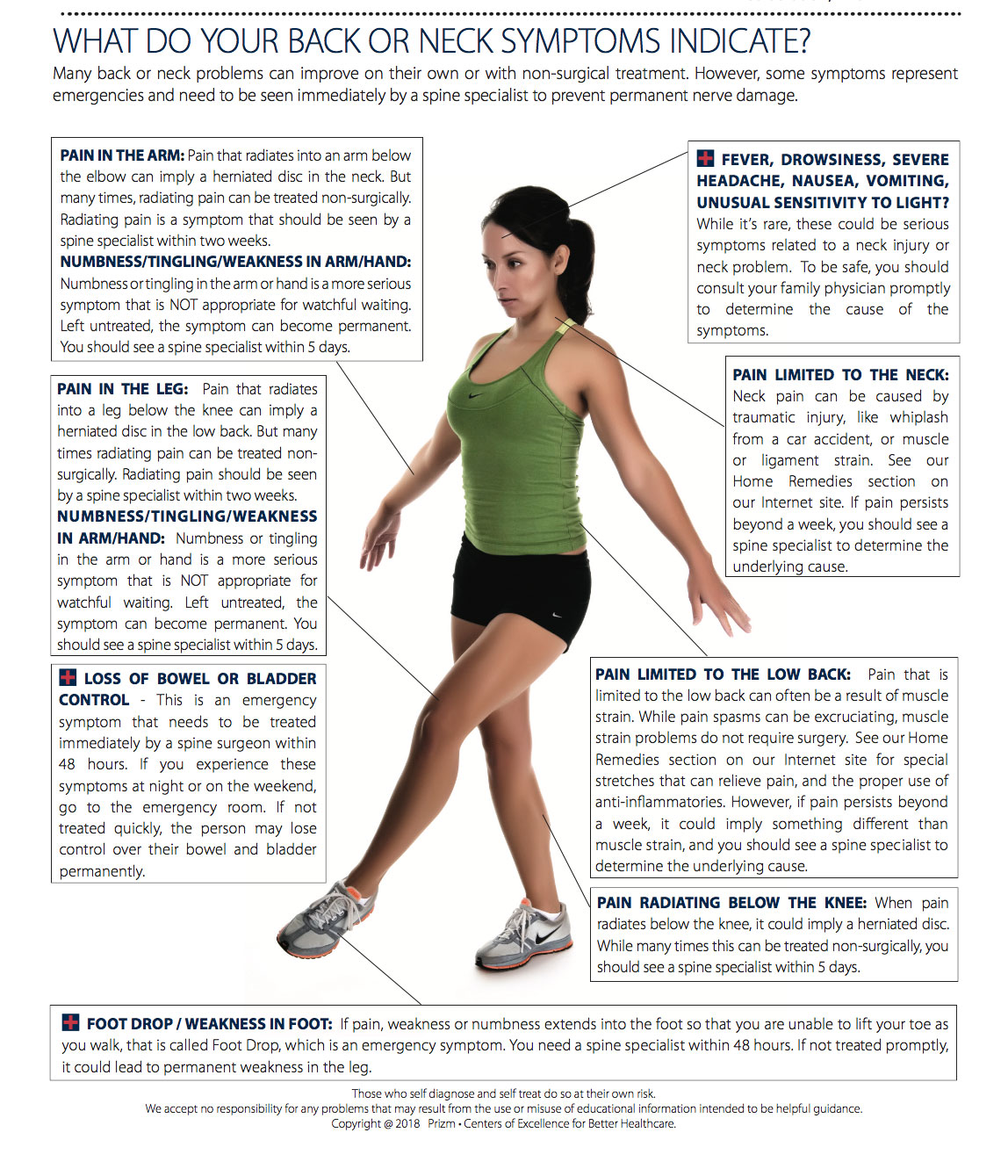
- Back and neck pain
- Pain radiating through an arm and/or leg
- Prominent lumps on the hands, feet or spine
- Numbness
- Burning
- Muscle cramps
[top]
Diagnosis
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
- Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment.
- Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
- X-rays are usually the first step in diagnostic testing methods. X-rays show bones and the space between bones. They are of limited value, however, since they do not show muscles and ligaments.
- MRI (magnetic resonance imaging) uses a magnetic field and radio waves to generate highly detailed pictures of the inside of your body. Since X-rays only show bones, MRIs are needed to visualize soft tissues like discs in the spine. This type of imaging is very safe and usually pain-free.
- CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
- Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
- Bone scan: Bone imaging is used to detect infection, malignancy, fractures and arthritis in any part of the skeleton. Bone scans are also used for finding lesions for biopsy or excision.
- Discography is used to determine the internal structure of a disc. It is performed by using a local anesthetic and injecting a dye into the disc under X-ray guidance. An X-ray and CT scan are performed to view the disc composition to determine if its structure is normal or abnormal. In addition to the disc appearance, your doctor will note any pain associated with this injection. The benefit of a discogram is that it enables the physician to confirm the disc level that is causing your pain. This ensures that surgery will be more successful and reduces the risk of operating on the wrong disc.
- Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.

[top]
Treatment
The goal when treating bone spurs is to minimize pain and prevent any additional joint damage. Treatment methods may include weight loss, stretching and physical therapy, rest and ice. Injections can reduce inflammation long enough to relieve symptoms. Medications such as ibuprofen or injections may be administered for pain. Bone spurs can be surgically removed in the case of serious damage and deformity.
[top]
FAQs
How can osteoporosis impact the spine and cause a bone spur?
Osteoporosis can have extremely serious consequences on the spine. It is a degenerative condition in which joint cartilage can begin to wear down, causing bone to rub against bone. As a result, the body may begin to produce new bone to protect against this, which is how a bone spur forms.
How can I tell if I have a bone spur?
Bone spurs can generally be detected through X-ray, which can provide a visual of any bony deposits.
Do I need surgery to treat a bone spur?
Because bone spurs are usually evidence of an underlying problem, this main problem should be addressed first. This can include treatment methods for degenerative disc disease, arthritis and osteoporosis. These conditions can often be successfully treated with nonsurgical methods.
[top]
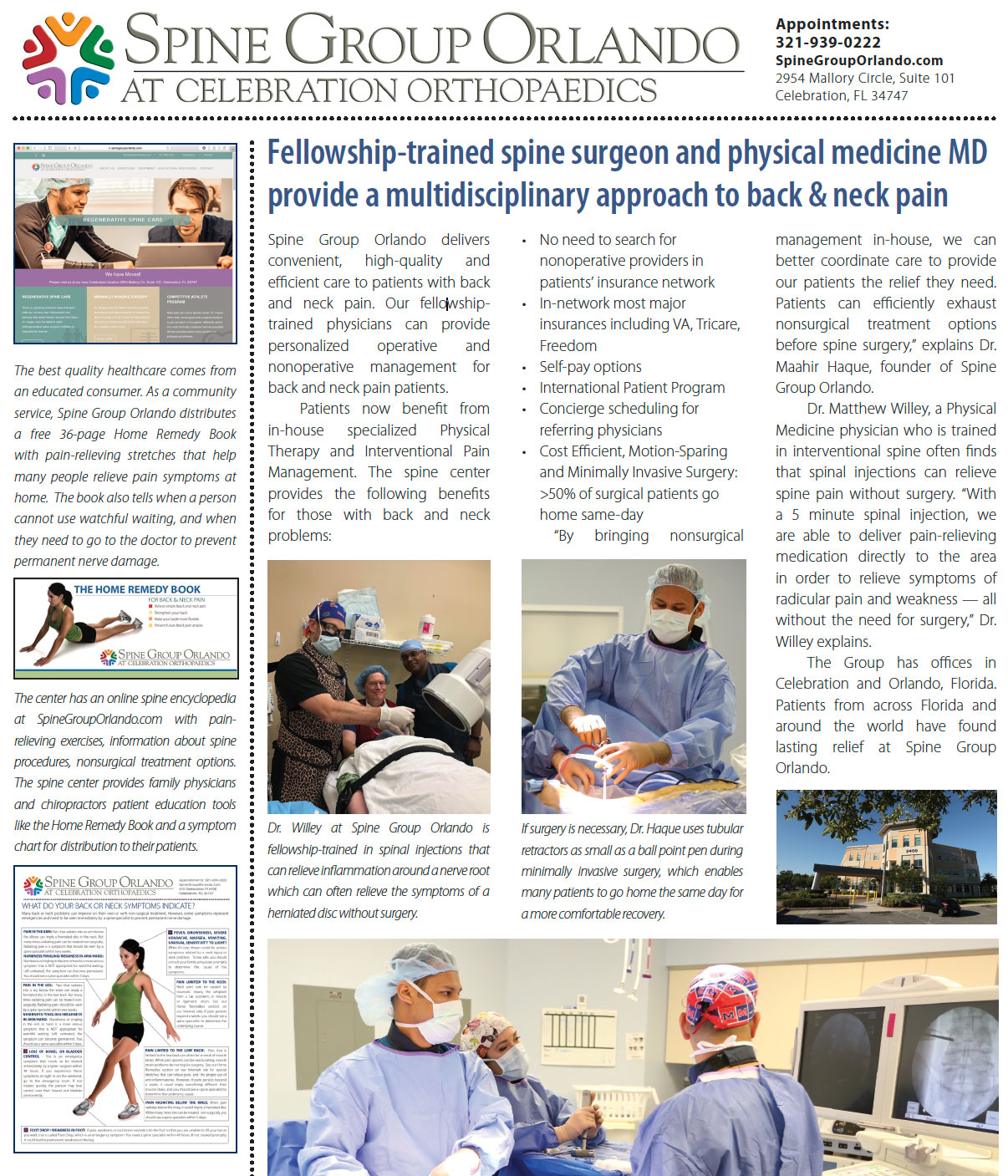
Maahir Haque, MD is recognized as a leader in the field of minimally invasive spine surgery. At Spine Group Orlando, Dr. Maahir Haque also provides second opinions for spine surgery and MRI reviews for those with back pain and neck pain. Dr. Haque emphasizes non-surgical options for back pain and neck pain where possible. This can include accessing a back pain specialist with expertise in pain-relieving spinal injections and spine therapists. Spine therapy can include back stretches that can be a future home remedy for back pain or neck pain. If spine surgery is necessary because of a herniated disc, spinal fracture, or spinal stenosis, Dr. Maahir Haque operates through tubular retractors that reduce the size of the incision, lessen blood loss, reduce time in the hospital, speed return to activity with a less painful recovery. This spine surgery expertise enables many patients to have outpatient spine surgery and be home the same day. Spine Group Orlando and Dr. Maahir Haque provides artificial disc replacement in the neck using the Mobi-C disc implant, the first FDA-approved disc for multiple levels in the neck. Prodisc-C is also used for artificial disc replacement in the cervical spine. Dr. Haque is also one of the few spine surgeons in Orlando, Florida to provide lumbar artificial disc replacement using the Prodisc-L artificial disc. Dr. Haque is also referred patients from across Orlando and north central Florida for artificial disc replacement surgery as an alternative to spinal fusion. Accordingly, Dr. Haque's patients travel from across north central Florida, including: Orlando; Jacksonville; Tallahassee; Lakeland; Gainesville; Tampa; Daytona Beach; and Cocoa Beach. The spine center, as a destination for medical tourism for some international patients from Mexico and the Caribbean, can provide recommendations to out-of-town patients on nearby hotels and tourist attractions. Dr. Haque is featured on the national site CentersforArtificialDisc.com as an author on the subject of artificial disc replacement for herniated discs in the neck. The Centers for Artificial Disc web site has content specific to disc replacement options and alternatives to spinal fusion. Click here to visit the Centers for Artificial Disc.