Orlando’s Lumbar Disc Replacement Specialist
Orlando’s Lumbar Disc Replacement Specialist
 About the Centinel Prodisc-L Artificial Disc
About the Centinel Prodisc-L Artificial Disc
The prodiscL has a very long clinical history (25+ years) and has been widely used throughout the world. Theprodisclineoftotaldiscreplacements (TDRs) are the most widely studied TDRs, with over400 peer-reviewed published studies, reporting on over 13,000 patients. The first implantation ofa prodiscL took place in 1990, and thesecondgeneration design received US PMA approval in 2006. The prodiscdesign has been validated with over 125,000 device implantations and a reported reoperation rate of less than 1%.
Each year in the U.S., more than 200,000 spinal fusion surgeries are performed to relieve excruciating pain caused by damaged discs in the low back and neck areas. Patients researching regional centers that are qualified to implant artificial discs are learning that there is great variation among spine surgeons in the type of discs used, and IF the doctor recommends any artificial disc surgery for a particular diagnosis.
It is important to remember that this technology is still evolving with new implants continually in development. Your spine surgeon is the best resource to discuss if it is appropriate for you, and what model of artificial disc is best suited for your case.
 The number and type of artificial discs available in the United States is expected to grow as new models emerge on the scene and surgeons become trained in their use. Each disc is designed for use either in the low back (lumbar area) or neck (cervical area).
The number and type of artificial discs available in the United States is expected to grow as new models emerge on the scene and surgeons become trained in their use. Each disc is designed for use either in the low back (lumbar area) or neck (cervical area).
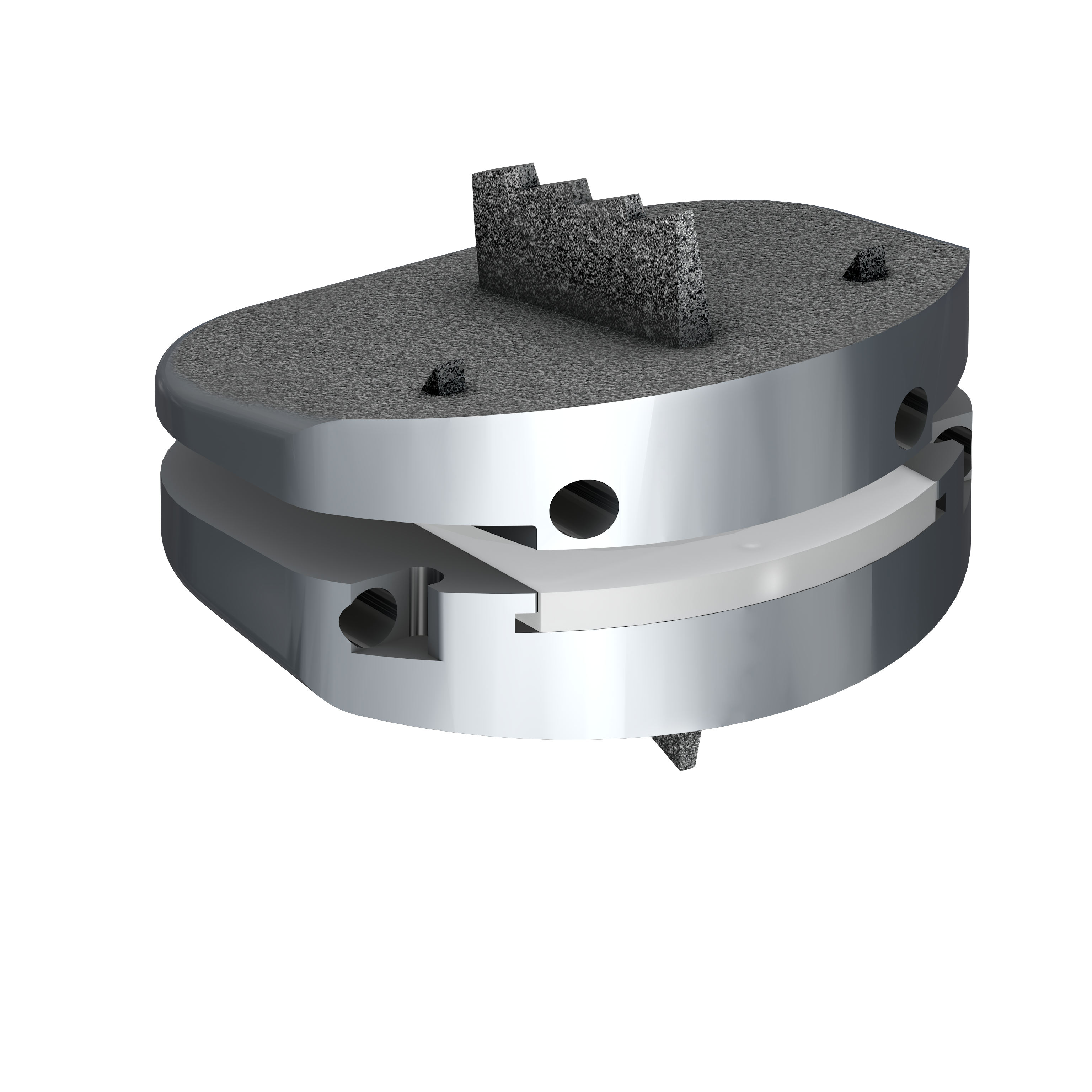
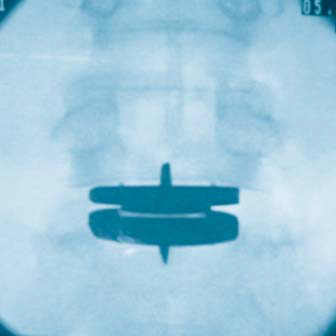
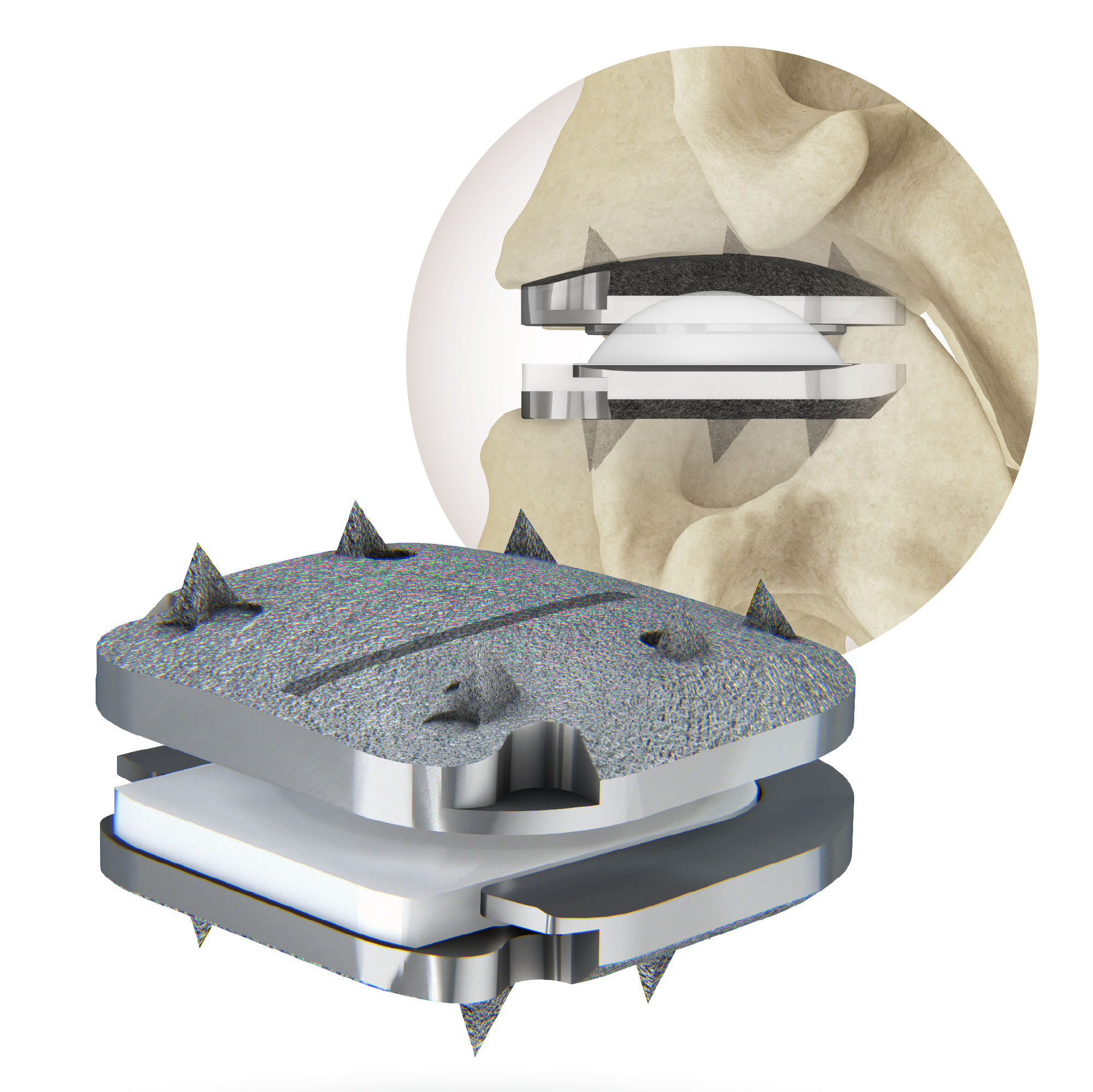
The Prodisc L is approved for one or two-level use in patients with single-level degenerative disc disease at either L3/L4, L4/L5 or L5/S1 who have failed at least six months of nonoperative care. It’s designed to help restore the natural distance between two vertebrae and the natural motion of the lumbar spine. It consists of three implant components; two metallic endplates and a plastic inlay.
Centinel Spine is currently the only company in the United States to offer Total Disc Replacement devices for both the cervical and lumbar spine.
An Alternative to Fusion Surgery
The artificial disc concept is intended to be an alternative for spinal fusion surgery. Each year in the U.S., more than 200,000 spinal fusion surgeries are performed to relieve excruciating pain caused by damaged discs in the low back and neck areas.
During a fusion procedure, the damaged disc is typically replaced with bone from a patient’s hip or from a bone bank. Fusion surgery causes two vertebrae to become locked in place, putting additional stress on discs above and below the fusion site, which restricts movement and can lead to further disc herniation with the discs above and below the degenerated disc. An artificial disc replacement is intended to duplicate the function level of a normal, healthy disc and retain motion in the spine.
When a natural disc herniates or becomes badly degenerated, it loses its shock-absorbing ability, which can narrow the space between vertebrae. In fusion surgery, the damaged disc isn’t repaired but rather is removed and replaced with bone that restores the space between the vertebrae. However, this bone locks the vertebrae into place, which can then damage other discs above and below.
A common aspect of all artificial discs is that they are designed to retain the natural movement in the spine by duplicating the rotational function of the discs Mother Nature gave us at birth. Most artificial disc designs have plates that attach to the vertebrae and a rotational component that fits between these fixation plates. These components are typically designed to withstand stress and rotational forces over long periods of time. Still, like any manmade material, they can be affected by wear and tear.
Benefits
Some of the main benefits of the artificial disc parallel that of knee replacement and hip replacement. This can include the following benefits:
- An artificial disc in the neck or back, in principle, is designed to retain motion in that particular segment of the spine.
- It prevents degeneration of disc levels above and below the affected disc
- There is no bone graft required
- There can be a quicker recovery and return to work or activity
- It can be a less invasive and less painful surgery than a fusion
- There can be less blood loss during surgery
Lumbar vs. Cervical Artificial Discs
Because of the weight of the body and the rotational stress that the trunk places on discs in the low back (lumbar) area, more stress is placed on artificial discs in the lumbar area than in the neck (cervical) area, which only supports the weight of the head.
A second issue relates to the ease of the artificial disc surgery and any necessary revision surgery to replace a worn out artificial disc. Because the surgeon must access the front of the spine, an incision is made in the abdomen for lumbar discs and in the front of the neck for cervical discs. Generally speaking, many spine surgeons believe access to the cervical discs can be easier than the lumbar discs.
Other issues to consider
When treating knee and hip replacement patients, orthopedic surgeons try to postpone the implantation of an artificial joint until a patient is at least 50 years old so that they do not outlive their artificial joint, which typically lasts anywhere from 15 to 20 years. Revision surgery, which may be necessary to replace a worn-out artificial joint, can be complex.
This is also a concern with the artificial disc. Unlike knee and hip replacement patients who are typically in their 50s or 60s, many patients can benefit from artificial disc technology at a much younger age — in their 20s or 30s. Therefore, the implantation of an artificial disc in younger patients can raise a surgeon’s concern about the potential life span of the artificial disc in the spine and the need for revision surgery to replace a worn-out artificial disc, which can be complex.
Frequently Asked Questions
Why the artificial disc is big news?
The artificial disc is projected to have a dramatic impact on the field of spine, just as the introduction of the artificial joint had for those with damaged knee or hip joints. Before the introduction of the artificial knee or artificial hip, these joints were fused. Fusion of a knee or hip today would be unthinkable, thanks to artificial knees and hips. Finally, this new technology is being brought to the field of spine.
Centinel offers the Prodisc-L (lumbar) and Prodisc-C (cervical), both are FDA approved for use in the United States. The Prodisc-L design is based on a ball and socket principle and is composed of three implant components, two metal endplates and a plastic inlay. The Prodisc-L implant materials are typically used in total joint replacement and have been used for at least two decades in spinal arthroplasty procedures. Patients suffering from symptomatic cervical disc disease at one level from C3 to C7 may benefit from ProDisc-C total disc replacement. The purpose of ProDisc-C artificial disc surgery is to remove the diseased disc, restore normal disc height and provide potential for motion at the disturbed segment.
What does FDA approval mean?
FDA approval typically comes after extensive clinical studies that compare a group of patients who requested an artificial disc, with a control group of patients with similar problems who received traditional fusion surgery.
In some studies, the percent of patients needing a second surgery was higher with traditional fusion than with artificial disc, implying that the new disc may have lower complications than fusion surgery.
Huge demand predicted for the disc
The arrival of the artificial disc is tremendous news because of the widespread incidence of degenerative disc disease. A natural by-product of aging occurs through the loss of resiliency in spinal discs and a greater tendency to herniate, especially when placed under a heavy load, like when we lift objects.
In the U.S., recent studies report that 56% of Americans are overweight, and 25% are obese, which only puts more stress on aging discs. Also some unfortunate people have a family history of degenerative disc disease, which increases their risk of developing it.
In any event, expectations of aging baby boomers — those born between 1946 and 1964 now in their fifties and sixties — are for an active rather than sedentary retirement.
All of these trends are creating tremendous demand for a technological advance that promises to restore motion to damaged and aging backs and necks.
How do artificial discs differ?
A common aspect of all artificial discs is that they are designed to retain the natural movement in the spine by duplicating the shock-absorbing and rotational function of the discs Mother Nature gave us at birth.
Most artificial disc designs have plates that attach to the vertebrae and a rotational component that fits between these fixation plates. These components are typically designed to withstand stress and rotational forces over long periods of time. Still, like any man made material, they can be affected by wear and tear.
 Current considerations include tiny shavings that may be produced by the component pieces as they wear on each other after implantation. Other considerations relate to surgeons perception of how easy a particular disc is to implant in the spine — as well as how easy it is to REMOVE. Some discs, for example, have characteristics that enable them to be easily tapped into place which then lock them in place. The problem is if that disc needs to be taken out, it’s extremely difficult.
Current considerations include tiny shavings that may be produced by the component pieces as they wear on each other after implantation. Other considerations relate to surgeons perception of how easy a particular disc is to implant in the spine — as well as how easy it is to REMOVE. Some discs, for example, have characteristics that enable them to be easily tapped into place which then lock them in place. The problem is if that disc needs to be taken out, it’s extremely difficult.
Consequently, manufacturers of artificial discs aim to design discs that are not only resistant to wearing out, but also easy to install and remove if revision surgery is needed. Doing all the above has proven to be a tall order.
Who is qualified to perform surgery?
Surgeons typically attend special courses conducted by the specific manufacturers of the various discs. The training is specific to the brand of artificial disc, because installation procedures and the instruments used vary slightly from disc to disc.
The dollars and cents of new technology
Not surprisingly, some health insurance companies are choosing to sit on the sidelines by refusing to pay for any artificial disc surgery, just like they refuse to pay for new drugs. Many health care providers see this only as just another tactic for certain insurance company to save expenses by restricting access to new advances for as long as they can argue the case.
Interestingly, however, some employers and workers compensation carriers in several states are endorsing artificial disc surgery and more than willing to pay for it. Why? Because historically fusion surgery has had such abysmal return to work rates among those who injure their backs on the job. From the employer’s perspective, those patients who have had fusion surgery are a lost cause. In their mind, artificial disc surgery is the best bet for getting the person back to the workplace.
The details about artificial disc technology
During a fusion procedure, the damaged disc is typically replaced with bone from a patient’s hip or from a bone bank, and locked in place with metal plates and screws. Fusion surgery locks two vertebrae in place, putting additional stress on discs above and below the fusion site, which restricts movement and can cause other discs to herniate.
An artificial disc replacement, however, is designed to duplicate the function level of a normal, healthy disc and retain motion in the spine. Some experts estimate that over the next 10 years, more than half of patients who would otherwise receive a fusion will receive an artificial disc instead. Educated consumers nationwide are expected to migrate to regional spine centers for access to this latest technological advance in spine care.
Most artificial disc designs have plates that attach to the vertebrae and a rotational component that fits between these fixation plates. These components are typically designed to withstand stress and rotational forces over long periods of time. Still, like any man-made material, they can be affected by wear and tear, and damage from excessive loads.
Key benefits of artificial discs:
- Retains movement of the vertebrae by replicating the function of a healthy disc.
- May prevent discs above and below from herniating in the future.
Key risks of artificial discs:
- The man-made disc might wear out over 10 years and need replacement.
- The load placed on the metal disc from the trunk (especially from overweight people) can accelerate wear and damage to the disc. The load place on neck discs, however, is viewed to be less.
- Revision surgery to replace the damaged artificial disc in the lumbar area is viewed by most surgeons as complex. Revision surgery on artificial discs in the neck is less complex.
- Risks of complications from surgeons who either have little training or experience in artificial disc.g or experience in artificial disc.
 Lumbar vs. cervical artificial discs
Lumbar vs. cervical artificial discs
Because of the weight of the body and the rotational stress that the trunk places on discs in the lumbar (low back) area, more stress is placed on artificial discs in the lumbar area vs. the cervical (neck) area, which only supports the weight of the head, explains Dr. Haque, who is Orlando’s Lumbar Disc Replacement Specialist. “I favor artificial disc for cervical use currently, because wear and tear on an artificial 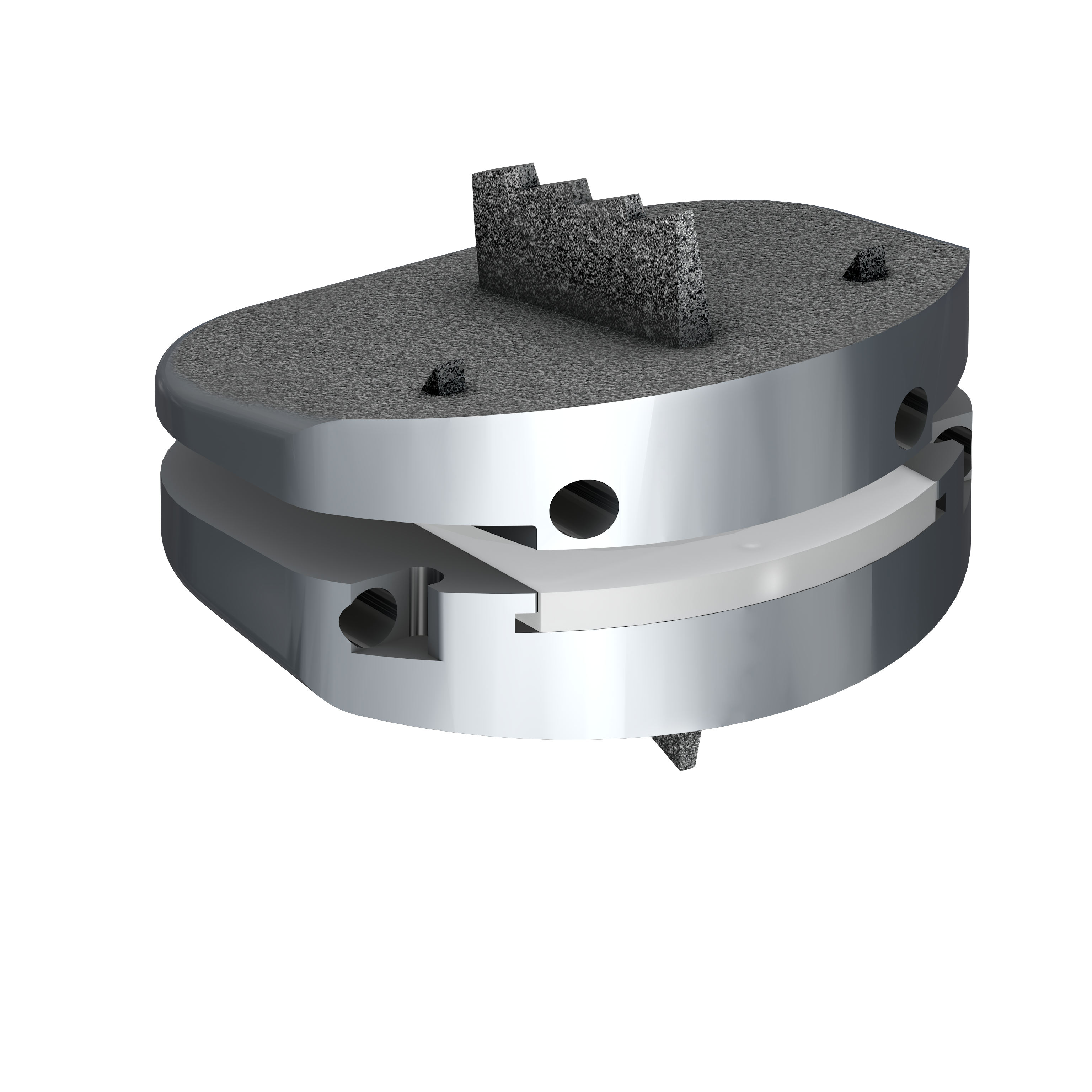 disc in the neck area is much less than a lumbar artificial disc. Secondly, the neck area is more accessible in surgery than the front of the lumbar spine. So even if a revision surgery were required, it would be easier to do on the neck than lumbar area. All of this underscores how important it is for the patient to be well informed. You need to ask how proficient is the surgeon at artificial disc surgery. How many have they done? Are they fellowship-trained?” Dr. Haque is
disc in the neck area is much less than a lumbar artificial disc. Secondly, the neck area is more accessible in surgery than the front of the lumbar spine. So even if a revision surgery were required, it would be easier to do on the neck than lumbar area. All of this underscores how important it is for the patient to be well informed. You need to ask how proficient is the surgeon at artificial disc surgery. How many have they done? Are they fellowship-trained?” Dr. Haque is
How does an artificial disc function?
When performing artificial disc replacement procedures for degenerative disc disease, Dr. Haque inserts a small prosthetic (artificial) disc comprising a polyethylene core that slides between two metal end plates. The end plates are attached to the vertebral body with anchoring teeth built along the rim of the end plates. The prosthetic discs replace the injured discs, helping to relieve chronic back pain. The polyethylene core allows movement of the spine, unlike fusions which prevent normal movement. The disc is made of the same material used in artificial hips and knees.
 In summary, some spine surgeons may be cautious about the use of artificial discs for the following reasons:
In summary, some spine surgeons may be cautious about the use of artificial discs for the following reasons:
- Wear and tear on artificial joints cant require revision surgery in 10 to 20 years that can be extremely complex.
- Most artificial disc implants only address rotational forces, not the up and down shock absorbing function of the natural disc.
- Overweight people can wear out a lumbar disc prematurely.
- New artificial discs are continually in development, however FDA approval is a lengthy process.
- There are not many 20-year-long studies that show the long-term effects of wear and tear on artificial disc implants.
Generally, the technology is very promising. Your spine surgeon can provide information if your problem can be addressed with this technology.
Due to the fact that the surgeon must access the front of the spine, an incision is made in the abdomen for lumbar discs and in the front of the neck for cervical discs. Typically, access to the cervical discs can be easier than the lumbar discs.
Maahir Haque, MD is recognized as a leader in the field of minimally invasive spine surgery. At Spine Group Orlando, Dr. Maahir Haque also provides second opinions for spine surgery and MRI reviews for those with back pain and neck pain. Dr. Haque emphasizes non-surgical options for back pain and neck pain where possible. This can include accessing a back pain specialist with expertise in pain-relieving spinal injections and spine therapists. Spine therapy can include back stretches that can be a future home remedy for back pain or neck pain. If spine surgery is necessary because of a herniated disc, spinal fracture, or spinal stenosis, Dr. Maahir Haque operates through tubular retractors that reduce the size of the incision, lessen blood loss, reduce time in the hospital, speed return to activity with a less painful recovery. This spine surgery expertise enables many patients to have outpatient spine surgery and be home the same day. Spine Group Orlando and Dr. Maahir Haque provides artificial disc replacement in the neck using the Mobi-C disc implant, the first FDA-approved disc for multiple levels in the neck. Prodisc-C is also used for artificial disc replacement in the cervical spine. Dr. Haque is also one of the few spine surgeons in Orlando, Florida to provide lumbar artificial disc replacement using the Prodisc-L artificial disc. Dr. Haque is also referred patients from across Orlando and north central Florida for artificial disc replacement surgery as an alternative to spinal fusion. Accordingly, Dr. Haque's patients travel from across north central Florida, including: Orlando; Jacksonville; Tallahassee; Lakeland; Gainesville; Tampa; Daytona Beach; and Cocoa Beach. The spine center, as a destination for medical tourism for some international patients from Mexico and the Caribbean, can provide recommendations to out-of-town patients on nearby hotels and tourist attractions. Dr. Haque is featured on the national site CentersforArtificialDisc.com as an author on the subject of artificial disc replacement for herniated discs in the neck. The Centers for Artificial Disc web site has content specific to disc replacement options and alternatives to spinal fusion. Click here to visit the Centers for Artificial Disc.