Injection Therapy
Injection Therapy
The philosophy of the spine care team at Spine Group Orlando is that many patients in our experience will get better with rest, medication or injections that reduces inflammation, core strengthening and spine-specialized physical therapy programs.
 Injection therapy is intended to be a means to an end. The goal is to provide the patient with enough pain relief to bridge from inactivity to physical therapy, where back problems can be better treated with special stretches and exercises.
Injection therapy is intended to be a means to an end. The goal is to provide the patient with enough pain relief to bridge from inactivity to physical therapy, where back problems can be better treated with special stretches and exercises.
If you haven’t tried non-surgical treatment options, you are likely pursuing a surgical path perhaps unnecessarily. In the field of spine, specialists use cortisone injections, epidural steroid injections, trigger point injections and nerve blocks to relieve pain in the spine.
Philosophically, Spine Group Orlando has a conservative approach to the care of his patients and encourages non-surgical treatment first. This is in contrast to many other spine surgeons who may be biased toward spine surgery because of their limited experience with non-surgical treatment options.
Spine Group Orlando refers patients to specialists who are proficient in spinal injections.
When those non-surgical options fail, or if there are emergency symptoms, then minimally invasive spine surgery is the next treatment option to explore.
Injections can be both therapeutic AND diagnostic
At Spine Group Orlando, the use of injection therapy accomplishes two very important functions.
THERAPEUTIC FUNCTION: The first purpose of the spinal injection is to provide a therapeutic benefit to the patient, that is, relief of pain symptoms, or relief of the weakness or numbness in the leg or arm caused by a herniated disc.
DIAGNOSTIC FUNCTION: The second function is to reveal important diagnostic information to the spine specialist. For instance, if the injection of medication near the nerve root at a certain level of the spine FAILS TO RELIEVE the pain symptom or the weakness caused by the impinged nerve, the spine surgeon learns something very important. One possibility is that the symptoms are coming from a different disc at a different level. This is key, because without this information, a surgeon could operate and remove disc tissue at a level that appears on an MRI to have a herniation, but in fact that herniation is NOT the cause of the patient’s symptoms.
Injections can ensure a successful surgery
Is is possible to be misled by an MRI that shows a disc herniation? Absolutely. Research studies have shown that about 40% of healthy people over age 40, with no back pain whatsoever, can have disc problems that would show up on an MRI.
Said another way, a herniated disc that appears on an MRI scan does not necessarily have to be the cause of one’s pain symptoms. It could be something else, like a disc problem at another level, an arthritic facet joint, a narrowing of the spinal canal (called stenosis) or other issue.
Injection therapy when done prudently, and not in a repetitious manner, can ensure that if surgery is necessary, the right surgery would be performed on the real problem.
If your surgeon did not explore injections, you could be having an unnecessary surgery, or a surgery at the wrong level
There are two worst-care scenarios that injection therapy is designed to prevent:
Prevent a person from having a surgery that wasn’t necessary in the first place.
Prevent a surgeon from operating on the wrong disc.
In conclusion, if your spine specialist doesn’t at least consider the role of injection therapy in your assessment and treatment, you may be at risk for one of the two worst-case scenarios.
Epidural steroid injections
An epidural steroid injection is done to help relieve the symptoms of nerve irritation or inflammation. The irritation or inflammation can occur for a number of reasons including bulging or herniated discs, arthritis and bone spurs that form in the back. Depending upon the nerve, or nerves, involved, patients may develop pain and/or other symptoms in different parts of the body. This could include numbness, tingling, and weakness. Irritation of the nerves in the neck may cause pain in the neck, shoulder and arm. Irritation of the nerves in the upper back may cause complaints in the back, sides, chest or abdomen. In the lower back, irritation or inflammation of the nerves can cause low back pain, buttock or leg pain.
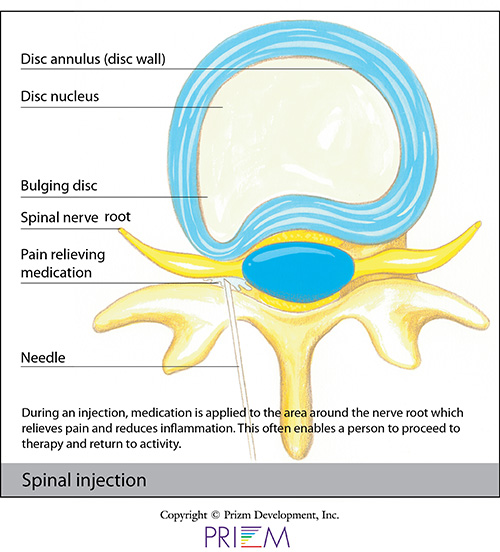
The nerves in the spine are covered by a thin membrane known as the dura. There is a space between the dura and the spinal canal called the epidural space. In an epidural spinal injection, the steroid medication is injected into this space.
Epidural steroid injections are most commonly performed as an outpatient procedure. Sometimes, though not always, an IV is started if medication for relaxation is to be administered. Patients are placed face down on a special x-ray table and the skin at the injection site is sterilely prepped. Numbing medication is then used to anesthetize the skin and tissue deep to the skin to make the procedure more comfortable. An x-ray machine called a fluoroscope is used to monitor placement of the epidural needle as well as where the medicine is being delivered. The procedure itself is relatively quick, taking approximately 20 minutes. Patients are monitored for a short time before being discharged home. On the day of the injection, patients are instructed not to drive and avoid strenuous activities. Some patients may experience a slight increase in pain for several days as the numbing medication wears off and while waiting for the steroid to work. The day following the injection, patients may return to their normal activities.
Epidural injections are not always beneficial. About half of the patients getting an epidural steroid injection will have relief of their pain. In some patients the relief may be substantial and long lasting. Some may only get partial relief and others may get no relief at all. If the first injection only gives partial relief, a second and, sometimes, a third injection may be recommended.
Facet Injection
The facet joints are small paired joints that act as hinges in our back, connecting all the vertebral bones yet still allowing us to bend and twist with ease. Sometimes, from injury or age, these joints can become irritated or they can develop arthritis and bone spurs, which makes movement painful. Depending on which joints are involved, symptoms of facet joint pain can include neck or shoulder pain, headaches, upper or lower back pain, hip, buttock or leg pain.
To relieve pain symptoms and restore range of motion, the spine physician may inject medication into or around the facet joints. The medicine injected into the facet joints can act like WD40 on a rusty door hinge, helping restore movement. Injections done around the facet joints are done to disable the sensory nerves (known as the Medial Branches) that go to the facet joints. If blocking the Medial Branch nerves is effective, a second procedure known as a Rhizotomy may be done to give a longer lasting benefit. Typically injections are done as a way to bridge the patient to therapy so the therapist can help the patient retain mobility after the effects of the medication wear off.
Facet injections are most commonly performed as an outpatient procedure. Sometimes, though not always, an IV is started if medication for relaxation is to be administered. Patients are placed face down on a special x-ray table and the skin at the injection site is sterilely prepped. Numbing medication is then used to anesthetize the skin and tissue deep to the skin to make the procedure more comfortable. An x-ray machine called a fluoroscope is used to monitor placement of the needle or probe as well as where the medicine is being delivered. These procedures are relatively quick, taking approximately 20 minutes. Patients are monitored for a short time before being discharged home. On the day of the injection, patients are instructed not to drive and avoid strenuous activities. Some patients may experience a slight increase in pain for several days as the numbing medication wears off and while waiting for the steroid to work. The day following the injection, patients may return to their normal activities. It is important, particularly in patients undergoing medical branch block procedures, to keep a pain diary in order to maintain an accurate measure of your response to the injection.
Trigger Point Injections
Trigger points are painful tissues in and around muscles. Pressure to the painful tissues can cause an aching or sharp pain sensation. Trigger point injections are the administration of a local anesthetic and steroid medication in the muscles where pain is occurring. The injection may relieve spasms of the muscle and may last from weeks to months.
Trigger point injections are performed as an outpatient procedure. The skin at the injection site is sterilely prepped and numbing medication may be used to anesthetize the skin and tissue deep to the skin to make the procedure more comfortable. Patients are monitored for a short time before being discharged home. On the day of the injection, patients are instructed to avoid strenuous activities. Some patients may experience a slight increase in pain for several days as the numbing medication wears off and while waiting for the steroid to work. The day following the injection, patients may return to their normal activities.
Sacro-Iliac Joint Injections
The sacro-iliac joints are two paired joints connecting the lower part of the spine to the pelvis and lower half of the body. The SI joints are very rigid, stable joints due to their bony structure and design as well as their very strong supporting ligaments. Inflammation, irritation and arthritic changes in one or the other joint can occur and cause lower back pain.

A long lasting steroid (cortisone) can be injected into the sacro-iliac joint to help decrease inflammation and/or swelling of tissue in the joint space. As a result, patients may experience reduced pain caused by inflammation of the joint. The procedure involves inserting a needle through the skin and deeper tissues into the SI joint. Sacro-iliac joint injections are not always beneficial but in some patients the relief may be substantial and long lasting. If only partial relief is obtained, a repeat injection may be performed.
Sacro-iliac joint injections are performed as an outpatient procedure. Sometimes, though not always, an IV is started if medication for relaxation is to be administered. Patients are placed face down on a special x-ray table and the skin at the injection site is sterilely prepped. Numbing medication is then used to anesthetize the skin and tissue deep to the skin to make the procedure more comfortable. An x-ray machine called a fluoroscope is used to monitor placement of the needle as well as where the medicine is being delivered. SI joint injections are relatively quick, taking approximately 20 minutes. Patients are monitored for a short time before being discharged home. On the day of the injection, patients are instructed not to drive and avoid strenuous activities. Some patients may experience a slight increase in pain for several days as the numbing medication wears off and while waiting for the injected steroid to work. The day following the injection, patients may return to their normal activities.
Rhizotomy
Rhizotomy is a procedure in which the physician may use heat or cold to intentionally damage the ability of a problematic nerve to telegraph pain signals to the brain. While pain signals serve to warn us about danger or injury, sometimes a nerve can end up in a "stuck" position, sending a continuous pain signal to the brain.
Prior to having Rhizotomy done, a diagnostic injection of local anesthetic has usually been done at the problematic area to prove that this is where the pain is coming from. This procedure is most commonly done for facet joint or sacro-iliac joint pain. Also known by names such as neuroablation or neurotomy, Rhizotomy is the surgical procedure to purposely inhibit the nerve's ability to transmit a pain signal. During the procedure, the spine surgeon can destroy the problematic nerve by cutting it or by using extreme heat or cold. This intentional "short circuit" can be temporary or permanent, depending upon the procedure.
Rhizotomy is most commonly performed as an outpatient procedure. Sometimes, though not always, an IV is started if medication for relaxation is to be administered. Patients are placed face down on a special x-ray table and the skin at the injection site is sterilely prepped. Numbing medication is then used to anesthetize the skin and tissue deep to the skin to make the procedure more comfortable. An x-ray machine called a fluoroscope is used to monitor placement of the probe. Patients are monitored for a short time before being discharged home. On the day of the injection, patients are instructed not to drive and avoid strenuous activities. The day following the injection, patients may return to their normal activities.
Risks of injections
Risks involved with spinal injections are minimal. Minor superficial infections are reported to occur in approximately 1% of all injections with severe or deep infections occurring in 0.1 to 0.01% of injections. Bleeding is rare, as is nerve damage but either can occur due to direct injury to a blood vessel or nerve. A puncture of the dura during an epidural steroid can occur and is estimated to happen in 1 in 200 procedures. Also, patients who are acutely ill or have an active infection may not be able to have a procedure done.
Important- Patients who are on any blood thinning medications, such as coumadin (warfarin), plavix (clopidogrel), lovenox (heparin) or aspirin may be able to have these procedures but they cannot be done while on these medications. You and your treating physician, as well as your primary care doctor or cardiologist, will help decide whether or not it is safe to come off of your blood thinners to have an injection.
[Top]
Maahir Haque, MD is recognized as a leader in the field of minimally invasive spine surgery. At Spine Group Orlando, Dr. Maahir Haque also provides second opinions for spine surgery and MRI reviews for those with back pain and neck pain. Dr. Haque emphasizes non-surgical options for back pain and neck pain where possible. This can include accessing a back pain specialist with expertise in pain-relieving spinal injections and spine therapists. Spine therapy can include back stretches that can be a future home remedy for back pain or neck pain. If spine surgery is necessary because of a herniated disc, spinal fracture, or spinal stenosis, Dr. Maahir Haque operates through tubular retractors that reduce the size of the incision, lessen blood loss, reduce time in the hospital, speed return to activity with a less painful recovery. This spine surgery expertise enables many patients to have outpatient spine surgery and be home the same day. Spine Group Orlando and Dr. Maahir Haque provides artificial disc replacement in the neck using the Mobi-C disc implant, the first FDA-approved disc for multiple levels in the neck. Prodisc-C is also used for artificial disc replacement in the cervical spine. Dr. Haque is also one of the few spine surgeons in Orlando, Florida to provide lumbar artificial disc replacement using the Prodisc-L artificial disc. Dr. Haque is also referred patients from across Orlando and north central Florida for artificial disc replacement surgery as an alternative to spinal fusion. Accordingly, Dr. Haque's patients travel from across north central Florida, including: Orlando; Jacksonville; Tallahassee; Lakeland; Gainesville; Tampa; Daytona Beach; and Cocoa Beach. The spine center, as a destination for medical tourism for some international patients from Mexico and the Caribbean, can provide recommendations to out-of-town patients on nearby hotels and tourist attractions. Dr. Haque is featured on the national site CentersforArtificialDisc.com as an author on the subject of artificial disc replacement for herniated discs in the neck. The Centers for Artificial Disc web site has content specific to disc replacement options and alternatives to spinal fusion. Click here to visit the Centers for Artificial Disc.